Indications
Laparoscopic tubal cannulation is indicated for women with:
- Blocked or partially obstructed fallopian tubes leading to infertility.
- Tubal blockages that prevent the passage of eggs from the ovaries to the uterus, hindering natural conception.
Preoperative Evaluation
Before undergoing laparoscopic tubal cannulation, patients typically undergo a comprehensive preoperative evaluation, including:
- Medical History Review: To understand past health issues and fertility concerns.
- Physical Examination: To assess overall health and suitability for surgery.
- Fertility Assessment: Including ovarian reserve testing and partner’s semen analysis.
- Imaging Studies: Such as hysterosalpingogram (HSG) or sonohysterogram to evaluate the extent and location of tubal blockages.
- Counseling: Discussing the procedure, risks, benefits, and alternatives, including the potential need for assisted reproductive technologies (ART) like in vitro fertilization (IVF).
Procedure
- Anesthesia: Laparoscopic tubal cannulation is performed under general anesthesia in an operating room equipped for laparoscopic surgery.
- Incisions: Several small (typically 0.5 to 1 cm) incisions are made in the abdomen, usually around the belly button and lower abdomen.
- Trocar Placement: Trocars (hollow tubes) are inserted through the incisions to provide access for the laparoscope and specialized instruments.
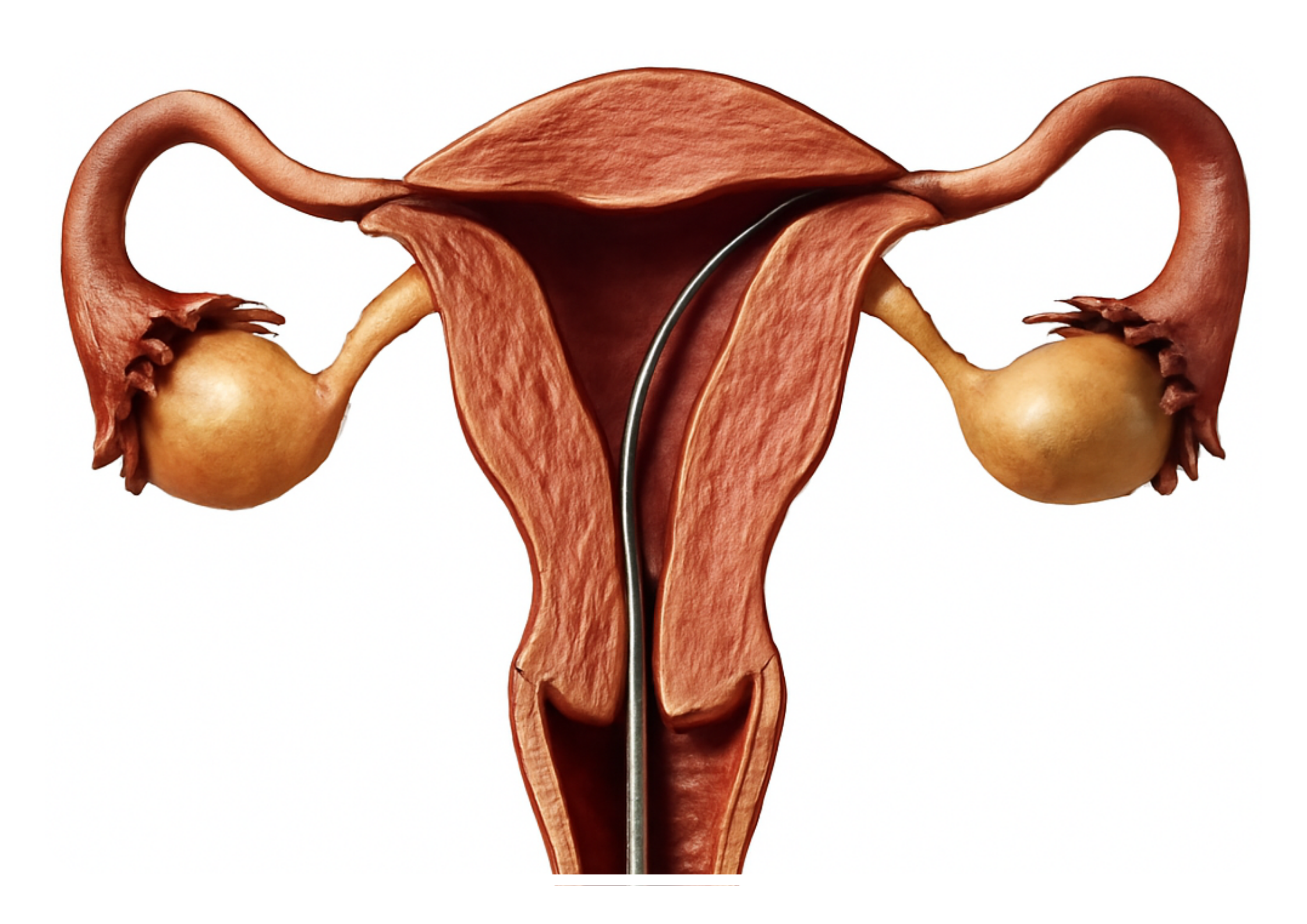
- Visualization: A laparoscope is inserted through one of the trocars to provide a magnified view of the pelvic organs, including the fallopian tubes. Carbon dioxide gas is used to inflate the abdominal cavity, creating space for visualization and instrument manipulation.
- Tubal Cannulation: Using specialized instruments such as catheters, guidewires, or microtools, the surgeon attempts to clear the blockage in the fallopian tubes. This may involve:
- Mechanical Dilation: A catheter is passed through the blockage to open the tube.
- Chemical Dissolution: A fluid is injected to dissolve the obstruction.
- Confirmation: After tubal cannulation is attempted, the patency of the fallopian tubes may be confirmed using dye (such as methylene blue) injected through the cervix and visualized as it passes through the fallopian tubes with the laparoscope.
- Closure: Once the procedure is completed, the instruments are removed, and the small incisions are closed with sutures or surgical glue. Dressings may be applied.
Success Rates
The success of laparoscopic tubal cannulation depends on various factors, including:
- The extent and location of tubal blockages.
- The cause of infertility.
- The patient’s age and overall fertility status.
Success rates for achieving pregnancy after tubal cannulation vary widely and may be influenced by factors such as tubal scarring or damage.
Considerations
- Alternative Treatments: In some cases, alternative fertility treatments such as IVF may be more appropriate or have higher success rates compared to tubal cannulation. The decision to undergo tubal cannulation should be made after careful consideration of all available treatment options and individual patient factors.
- Risks and Complications: Laparoscopic tubal cannulation carries risks similar to those of other laparoscopic surgeries, including bleeding, infection, injury to surrounding structures, and failure to achieve pregnancy. Patients should be informed about these risks during preoperative counseling.
- Fertility Counseling: Patients undergoing tubal cannulation should receive fertility counseling both before and after the procedure to discuss expectations, follow-up care, and the possibility of alternative treatments if tubal cannulation is unsuccessful.
Conclusion
Laparoscopic tubal cannulation is a potential option for women with blocked or partially obstructed fallopian tubes who are experiencing infertility. When performed by experienced surgeons in appropriately selected patients, tubal cannulation may offer the possibility of improved fertility and natural conception. However, success rates can vary, and patients should be counseled regarding the potential risks, benefits, and alternatives to the procedure.