Indications
Hysteroscopic polypectomy is indicated for women with symptomatic uterine polyps or those with polyps detected during diagnostic hysteroscopy for abnormal uterine bleeding, infertility, or other gynecological concerns. Symptoms associated with uterine polyps may include abnormal uterine bleeding (menorrhagia, metrorrhagia), intermenstrual bleeding, pelvic pain, or infertility.
Preoperative Evaluation
Before undergoing hysteroscopic polypectomy, patients typically undergo a preoperative evaluation, which may include:
- Pelvic Examination: To assess the overall reproductive health.
- Imaging Studies: Such as transvaginal ultrasound or saline infusion sonohysterography to visualize the polyps.
- Laboratory Tests: As needed, to evaluate overall health and readiness for surgery.
- Preoperative Counseling: To discuss the procedure, risks, benefits, and alternatives, and to address patient concerns.
Procedure
- Anesthesia: Hysteroscopic polypectomy is usually performed under local or general anesthesia, depending on the patient's preference, the complexity of the procedure, and the surgeon's preference.
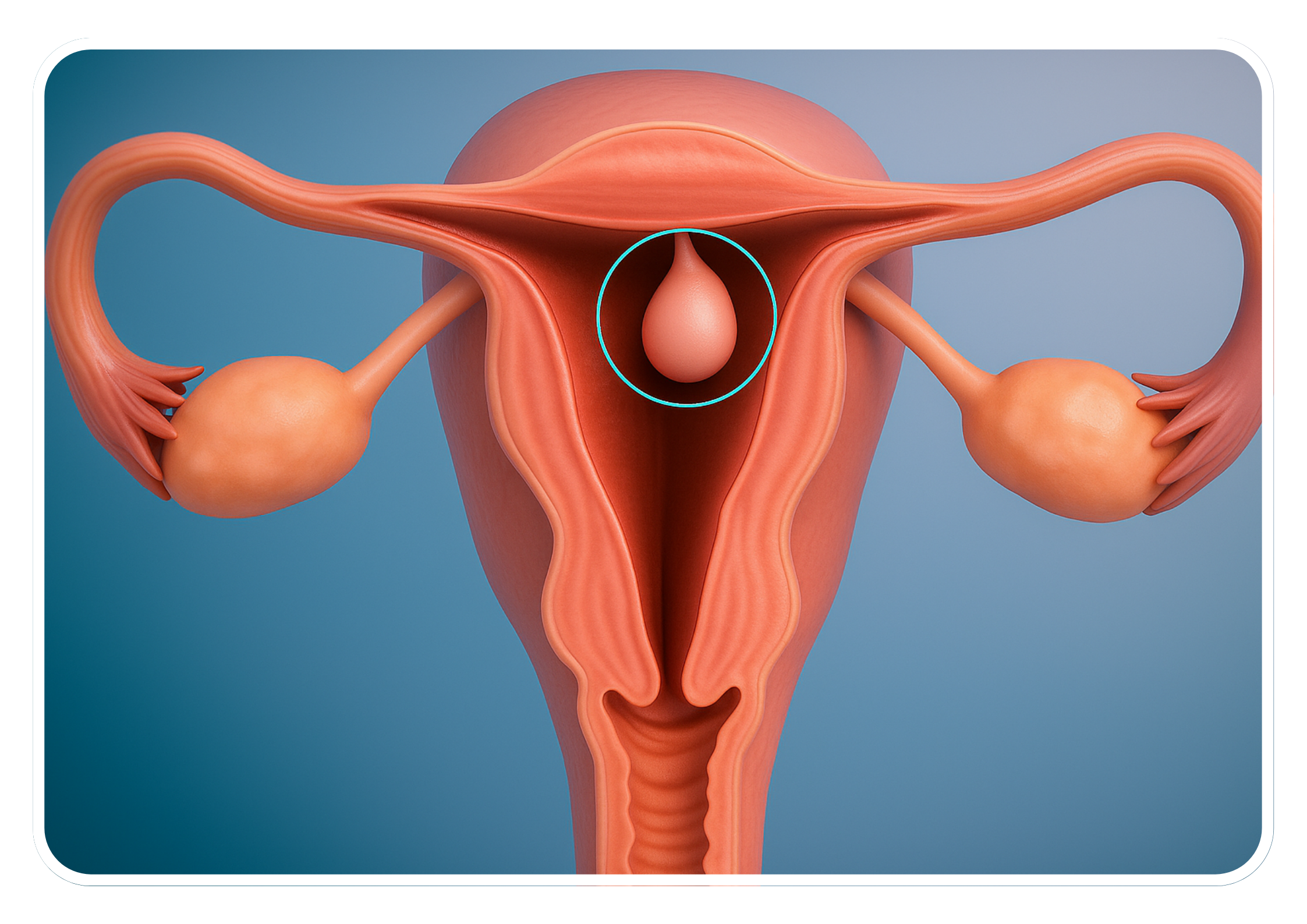
- Hysteroscope Insertion: A hysteroscope is inserted through the vagina and cervix into the uterine cavity, allowing visualization of the uterine lining and polyps. A saline solution may be used to distend the uterine cavity for better visualization.
- Polyp Removal: Specialized instruments, such as grasping forceps, scissors, or a resectoscope (a hysteroscopic instrument with an electrical wire loop), are passed through the hysteroscope to grasp, cut, or vaporize the polyps. The polyps are carefully removed from the uterine lining without damaging surrounding tissue.
- Inspection and Hemostasis: After polyp removal, the uterine cavity is inspected to ensure complete removal of all polyps and to identify any bleeding sites. Hemostasis (control of bleeding) is achieved using electrocautery, bipolar energy, or other hemostatic techniques.
- Closure: Once the procedure is completed, the hysteroscope is removed, and the vagina and cervix are inspected for any signs of injury or bleeding. No sutures are typically required, as the procedure is minimally invasive and does not involve abdominal incisions.
Advantages
- Minimally Invasive: Hysteroscopic polypectomy does not require abdominal incisions, resulting in less postoperative pain, shorter recovery times, and reduced risk of complications compared to traditional open surgery.
- Preservation of Fertility: The procedure allows for the removal of uterine polyps while preserving the uterus and fertility, making it an attractive option for women who desire future pregnancy.
- High Success Rate: Hysteroscopic polypectomy is associated with a high success rate in the removal of uterine polyps and improvement of associated symptoms, such as abnormal uterine bleeding or infertility.
Considerations
- Concurrent Procedures: In some cases, hysteroscopic polypectomy may be combined with other hysteroscopic procedures, such as endometrial ablation for treatment of abnormal uterine bleeding or diagnostic hysteroscopy for further evaluation of uterine pathology.
- Postoperative Care: After hysteroscopic polypectomy, patients may experience mild cramping, spotting, or vaginal discharge, which typically resolves within a few days. Follow-up appointments may be scheduled to monitor recovery and assess treatment outcomes.
- Risks and Complications: While hysteroscopic polypectomy is generally considered safe, potential risks and complications may include bleeding, infection, uterine perforation, or fluid overload from the distension media (saline solution). These risks are typically low but should be discussed with the patient during preoperative counseling.
Conclusion
Hysteroscopic polypectomy is a safe and effective procedure for the removal of uterine polyps, offering the advantages of minimally invasive surgery, preservation of fertility, and high success rates in symptom improvement. When performed by experienced gynecologists in appropriately selected patients, hysteroscopic polypectomy can provide significant relief of symptoms and improve reproductive outcomes. At Bliss IVF, we ensure that our patients receive the highest standard of care, tailored to their specific needs and conditions, providing comprehensive support throughout their treatment journey.