Indications
Combined diagnostic hysteroscopy-laparoscopy may be recommended for various gynecological indications, including:
- Evaluation of Infertility: Assessing the patency of the fallopian tubes, detecting uterine abnormalities (such as polyps, fibroids, or adhesions), and identifying pelvic factors contributing to infertility.
- Investigation of Abnormal Uterine Bleeding: Identifying intrauterine lesions, such as polyps or submucosal fibroids, and evaluating the endometrial cavity for abnormalities or pathology.
- Diagnosis of Pelvic Pain: Assessing for causes of pelvic pain, such as endometriosis, pelvic adhesions, ovarian cysts, or pelvic inflammatory disease.
- Suspected Uterine or Pelvic Pathology: Investigating suspected uterine abnormalities, such as congenital anomalies, uterine septum, or intrauterine adhesions (Asherman's syndrome).
Procedure
Combined diagnostic hysteroscopy-laparoscopy is typically performed under general anesthesia in an operating room equipped for both hysteroscopy and laparoscopy. The procedure involves the following steps:
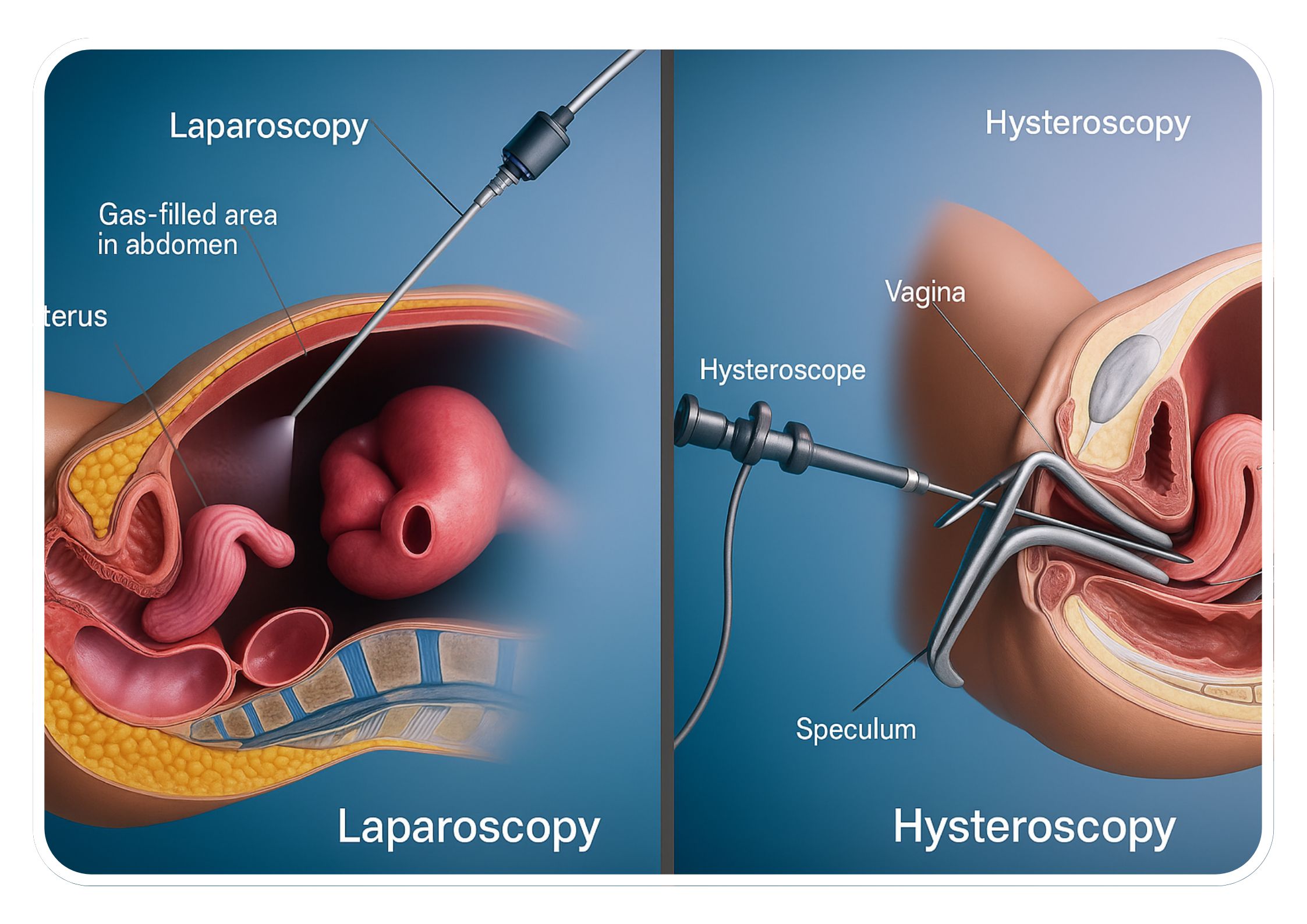
1. Hysteroscopy
- Insertion: A hysteroscope (a thin, lighted tube with a camera) is inserted through the cervix into the uterine cavity.
- Visualization: Saline may be used to distend the uterine cavity for better visualization.
- Assessment: Direct visualization of the endometrial lining, uterine cavity, and cervical canal to identify abnormalities such as polyps, fibroids, adhesions, or congenital anomalies.
2. Laparoscopy
- Insertion: A laparoscope (a thin, lighted tube with a camera) is inserted through a small incision near the umbilicus or lower abdomen.
- Inflation: Carbon dioxide gas is used to inflate the abdominal cavity, providing a clear view of the pelvic anatomy.
- Assessment: Visualization of the pelvic organs, including the uterus, fallopian tubes, ovaries, and surrounding structures to assess for signs of endometriosis, ovarian cysts, pelvic adhesions, or other pathologies.
3. Evaluation
- Intrauterine Assessment: Examination of the uterine cavity for abnormalities such as polyps, fibroids, adhesions, or congenital anomalies.
- Pelvic Assessment: Examination of the pelvic organs for signs of endometriosis, ovarian cysts, pelvic adhesions, or other pathologies.
4. Intervention (if necessary)
- Therapeutic Interventions: If abnormalities are detected, procedures such as polypectomy, myomectomy, adhesiolysis, or ovarian cystectomy may be performed laparoscopically or hysteroscopically, depending on the findings and clinical indications.
5. Closure
- Completion: The instruments are removed, and the incisions are closed with sutures or surgical glue.
- Postoperative Care: Dressings may be applied, and the patient is typically monitored in the recovery area before being discharged home.
Advantages
- Comprehensive Evaluation: Allows for a thorough assessment of both intrauterine and pelvic pathology in a single procedure.
- Minimally Invasive: Smaller incisions, less postoperative pain, reduced blood loss, and shorter recovery times compared to traditional open surgery.
- Accurate Diagnosis: Direct visualization of the pelvic anatomy and pathology allows for accurate diagnosis and targeted treatment of gynecological conditions contributing to infertility, abnormal uterine bleeding, or pelvic pain.
Considerations
- Patient Selection: Generally performed in appropriately selected patients based on clinical indications and diagnostic goals. Patients should undergo preoperative evaluation and counseling to discuss the risks, benefits, and alternatives to the procedure.
- Surgical Expertise: Requires specialized training and expertise in both hysteroscopy and laparoscopy. Surgeons should be proficient in minimally invasive surgical techniques and familiar with the nuances of combined diagnostic procedures.
Conclusion
Combined diagnostic hysteroscopy-laparoscopy is a valuable diagnostic tool in gynecology, providing clinicians with detailed information about intrauterine and pelvic pathology. By allowing for accurate diagnosis and targeted treatment, this minimally invasive procedure can help improve patient outcomes and facilitate appropriate management of gynecological conditions.
At Bliss IVF, our team of skilled surgeons and healthcare providers is dedicated to offering the highest standard of care. We are committed to helping you understand your treatment options and guiding you through your diagnostic journey with expertise and compassion.